How Immune Fatigue And Prescription Drug Abuse Impacts Long Term Health In Active Adults
Published on December 16, 2025
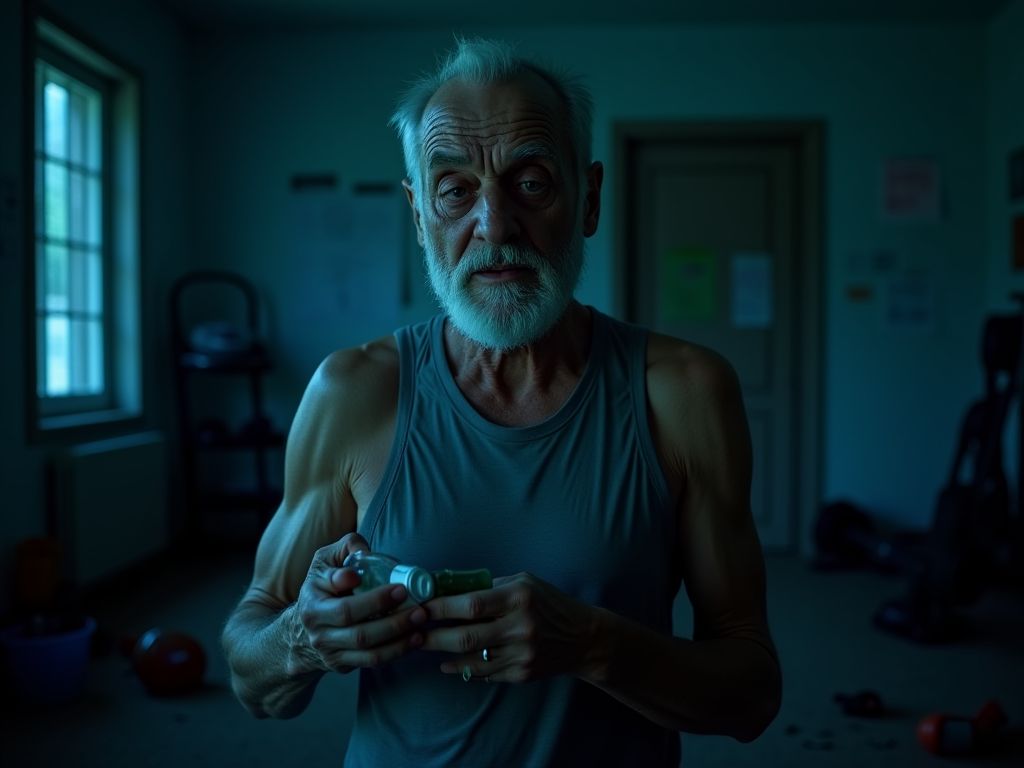
Understanding the Intersection of Immune Fatigue and Prescription Drug Abuse in Active Adults
Active adults—those who engage in regular physical activity, whether for fitness, sport, or recreation—are often seen as paragons of health. However, the demands of maintaining an active lifestyle can sometimes lead to unintended consequences, including immune fatigue and the misuse of prescription medications. Together, these factors can create a dangerous cycle that compromises long-term health. This article explores how immune fatigue and prescription drug abuse intersect, their individual and combined impacts on the body, and strategies to mitigate risks.
What Is Immune Fatigue?
Immune fatigue refers to a weakened state of the immune system, characterized by reduced effectiveness in defending against pathogens and slower recovery from illness. It can result from chronic stress, overtraining, inadequate sleep, poor nutrition, or prolonged exposure to environmental toxins. For active adults, intense physical training without sufficient recovery can trigger immune fatigue, making them more susceptible to infections, delayed wound healing, and increased inflammation.
The Rise of Prescription Drug Abuse Among Active Adults
Prescription drug abuse—defined as the misuse or overuse of medications such as opioids, stimulants, or anxiolytics—is a growing concern among active adults. Many turn to these drugs to manage pain from injuries, enhance performance, or cope with the mental stress of training. However, prolonged use or misuse can lead to dependency, organ damage, and long-term health complications.
How Immune Fatigue and Drug Abuse Interact
When immune fatigue and prescription drug abuse occur simultaneously, their combined effects can be particularly detrimental. For example, opioids and stimulants can suppress immune function, while chronic drug use may exacerbate inflammation and oxidative stress. This synergy increases the risk of infections, chronic diseases, and even premature aging.
Physical Health Consequences
The physical toll of immune fatigue and drug abuse is profound. Immune fatigue can lead to frequent illnesses, while drug abuse may cause organ damage (e.g., liver or kidney failure), cardiovascular strain, and musculoskeletal issues. Active adults may experience delayed recovery from injuries, increased susceptibility to injuries, and a higher incidence of chronic conditions like arthritis or diabetes.
Mental Health Implications
Mental health is often overlooked in discussions about immune fatigue and drug abuse. Chronic stress and immune dysfunction can contribute to anxiety, depression, and cognitive decline. Meanwhile, prescription drug abuse—especially with substances like benzodiazepines or stimulants—can worsen mental health, leading to dependency, mood swings, and even psychosis.
Cardiovascular Risks
Both immune fatigue and prescription drug abuse place significant strain on the cardiovascular system. Immune fatigue is linked to chronic inflammation, which accelerates atherosclerosis and increases the risk of heart disease. Stimulant abuse can cause hypertension, arrhythmias, and heart failure, while opioids may lead to respiratory depression and reduced cardiac output.
Metabolic Disruptions
Immune fatigue and drug abuse can disrupt metabolic processes, leading to insulin resistance, weight gain, and hormonal imbalances. For example, chronic inflammation from immune fatigue can impair glucose metabolism, while stimulant use may increase cortisol levels, promoting fat storage and metabolic syndrome.
Musculoskeletal Complications
Active adults often rely on their musculoskeletal system for performance, but immune fatigue and drug abuse can undermine its integrity. Immune fatigue may slow tissue repair, while drugs like corticosteroids (used for pain management) can weaken bones and muscles. Over time, this combination increases the risk of fractures, osteoporosis, and chronic pain.
Long-Term Health Risks and Mortality
The long-term consequences of immune fatigue and prescription drug abuse are severe. These include increased mortality rates from heart disease, cancer, and infectious diseases. Additionally, the cumulative effects of these factors can reduce life expectancy, diminish quality of life, and lead to costly healthcare burdens.
Frequently Asked Questions
- Can immune fatigue be reversed? Yes, with proper rest, nutrition, and stress management, immune function can often be restored.
- Is prescription drug abuse common among athletes? Yes, particularly in sports where pain management is prioritized over long-term health.
- How can active adults avoid immune fatigue? Prioritize sleep, manage training intensity, and maintain a balanced diet rich in antioxidants and nutrients.
- Are there safe alternatives to prescription drugs for pain management? Yes, including physical therapy, acupuncture, and natural supplements like turmeric or omega-3s.
- What should someone do if they suspect drug abuse? Seek help from a healthcare provider, addiction specialist, or support group immediately.
Conclusion: Prioritizing Holistic Health for Active Adults
Immune fatigue and prescription drug abuse are not isolated issues; they are interconnected challenges that demand a holistic approach to health. For active adults, the key to long-term well-being lies in balancing physical exertion with recovery, avoiding the misuse of medications, and seeking support when needed. By addressing these issues proactively, active adults can protect their health, sustain their performance, and enjoy a vibrant, active lifestyle for years to come.
Scientific References & Medical Evidence
- "Greater fatigue, disturbed sleep, persistent memory problems, and reduced CD4(+) T cell and B cell percentages in adults with a history of methamphetamine dependence." (2025) View study on PubMed.gov →
- "Tryptophan metabolism in post-withdrawal alcohol-dependent patients." (2014) View study on PubMed.gov →
CureCurious verifies facts through peer-reviewed research.
You might also like
Recommended for your journey
We've handpicked this top-rated health tool to help you achieve the results discussed in this article.
Check Price on Amazon*As an Amazon Associate, CureCurious.com earns from qualifying purchases. This helps us keep our research free for everyone.

Written by Dr. Sarah Mitchell
Nutrition Expert & MD
"Dr. Sarah Mitchell is a board-certified nutritionist with over 15 years of experience in clinical dietetics. She specializes in metabolic health and gut microbiome research."



