Why Silent Hypertension And Alcohol Consumption Is More Dangerous Than Most People Think
Published on December 15, 2025
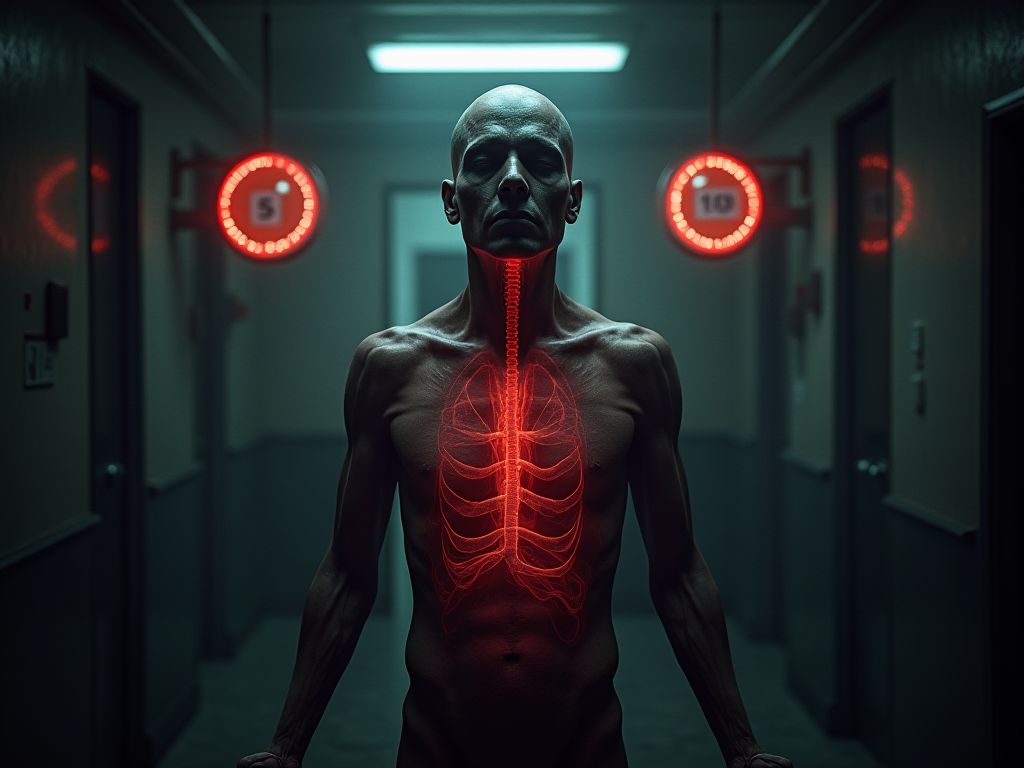
Why Silent Hypertension and Alcohol Consumption Are a Deadly Combination
High blood pressure, or hypertension, is often called the "silent killer" because it typically presents no symptoms until it causes severe complications. But when combined with alcohol consumption—a factor many underestimate—the risks become even more alarming. Silent hypertension, a condition where elevated blood pressure goes undetected, paired with alcohol’s detrimental effects on cardiovascular health, creates a dangerous synergy that can lead to life-threatening consequences. This article explores why this combination is more hazardous than most people realize and what you can do to protect your health.
1. Silent Hypertension: The Invisible Threat
Silent hypertension occurs when blood pressure is consistently high, but individuals experience no obvious symptoms. According to the American Heart Association, up to 40% of people with hypertension are unaware they have it. This lack of awareness delays treatment, allowing damage to organs like the heart, kidneys, and brain to progress silently.
- Mechanism: High blood pressure damages arteries over time, increasing the risk of heart disease, stroke, and kidney failure.
- Why it’s dangerous: Without symptoms, individuals may not seek medical care, leading to irreversible organ damage.
2. Alcohol’s Role in Raising Blood Pressure
Even moderate alcohol consumption can elevate blood pressure. Studies show that drinking more than two alcoholic drinks per day increases the risk of hypertension by up to 50%. Alcohol causes blood vessels to constrict, raises heart rate, and disrupts the balance of fluids in the body, all of which contribute to higher blood pressure.
Alcohol also interferes with the production of nitric oxide, a molecule that helps blood vessels relax, further exacerbating hypertension.
3. The Synergistic Effect of Alcohol and Silent Hypertension
When alcohol is consumed in combination with silent hypertension, the risks multiply. Alcohol’s ability to impair blood vessel function and increase heart rate can push already elevated blood pressure to dangerous levels, increasing the likelihood of heart attack, stroke, or kidney failure.
Moreover, alcohol can mask symptoms of hypertension, making it even harder to detect without regular blood pressure checks.
4. Long-Term Cardiovascular Damage
Chronic alcohol use combined with untreated hypertension accelerates atherosclerosis—the buildup of plaque in arteries. This process is a major contributor to heart disease and peripheral artery disease. Over time, the heart must work harder to pump blood, leading to heart failure.
Studies have shown that heavy drinkers with hypertension are twice as likely to develop coronary artery disease compared to non-drinkers.
5. Increased Stroke Risk
Alcohol consumption raises the risk of both ischemic and hemorrhagic strokes. Silent hypertension, by damaging blood vessels and increasing clotting risk, further elevates this danger. The combination can lead to strokes that are more severe and less likely to be survivable.
Research from the *Journal of the American Medical Association* links heavy drinking to a 30% higher stroke risk, especially in those with undiagnosed hypertension.
6. Kidney Damage and Alcohol
The kidneys rely on healthy blood pressure to filter waste from the blood. Silent hypertension can impair kidney function over time, while alcohol increases the risk of kidney disease by causing dehydration, elevating uric acid levels, and promoting inflammation.
Combining these factors can lead to chronic kidney disease or even kidney failure, particularly in individuals with diabetes or existing kidney issues.
7. Alcohol’s Impact on Medication Effectiveness
Alcohol can interfere with blood pressure medications, reducing their effectiveness. For example, it may counteract the benefits of ACE inhibitors or beta-blockers. Additionally, alcohol increases the risk of side effects from these medications, such as dizziness and liver damage.
This interaction can lead to uncontrolled hypertension and a higher risk of complications.
8. The Role of Oxidative Stress
Both alcohol and hypertension contribute to oxidative stress, a process where free radicals damage cells. This stress accelerates aging, damages blood vessels, and increases inflammation. Over time, it can lead to conditions like metabolic syndrome and type 2 diabetes, which further worsen hypertension.
Studies show that even moderate alcohol consumption can increase oxidative stress markers in the body.
9. Alcohol and the Risk of Hypertensive Crisis
A hypertensive crisis occurs when blood pressure rises to dangerously high levels (≥180/120 mmHg), potentially causing organ damage. Alcohol can trigger such crises, especially in individuals with untreated hypertension. Symptoms include severe headache, chest pain, and vision changes, but many people may not recognize these warning signs.
Without immediate medical intervention, a hypertensive crisis can be fatal.
10. The Hidden Cost of Alcohol-Induced Hypertension
Beyond the physical risks, alcohol-related hypertension can lead to significant financial and emotional burdens. Medical costs for complications like heart disease, stroke, or kidney failure can be overwhelming. Additionally, the psychological toll of living with a chronic condition and its potential consequences can be devastating.
Prevention through lifestyle changes and early detection is the most cost-effective solution.
Frequently Asked Questions
Q: Is any amount of alcohol safe for people with hypertension?
A: Even moderate drinking (e.g., one drink per day for women, two for men) can raise blood pressure. The American Heart Association recommends limiting alcohol to reduce risk.
Q: Can quitting alcohol reverse hypertension?
A: While quitting alcohol can lower blood pressure and improve overall health, it may not reverse existing damage. However, it significantly reduces the risk of complications.
Q: How can I tell if I have silent hypertension?
A: Regular blood pressure checks are the only way to detect silent hypertension. If you have risk factors like family history, obesity, or a sedentary lifestyle, consult a healthcare provider.
Conclusion
The combination of silent hypertension and alcohol consumption is a hidden but deadly health risk. By understanding how these factors interact, individuals can take proactive steps to monitor their blood pressure, limit alcohol intake, and seek medical care when needed. Early detection and lifestyle changes are crucial to preventing the severe complications associated with this dangerous pairing. Your health is worth the effort—don’t wait until it’s too late.
Scientific References & Medical Evidence
- "Alcohol intake masked the protective effects of tea consumption against all-cause mortality and blood pressure progression: Findings from CHNS cohort, 1993-2011." (2023) View study on PubMed.gov →
- "Alcohol, tobacco, and hypertension." (1982) View study on PubMed.gov →
CureCurious verifies facts through peer-reviewed research.
You might also like
Recommended for your journey
We've handpicked this top-rated health tool to help you achieve the results discussed in this article.
Check Price on Amazon*As an Amazon Associate, CureCurious.com earns from qualifying purchases. This helps us keep our research free for everyone.

Written by Dr. Sarah Mitchell
Nutrition Expert & MD
"Dr. Sarah Mitchell is a board-certified nutritionist with over 15 years of experience in clinical dietetics. She specializes in metabolic health and gut microbiome research."



